Interleukin 24 (IL-24) to treat inflammatory diseases
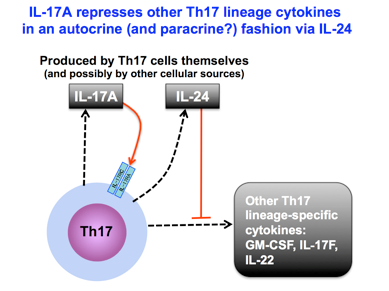
Proinflammatory T-helper 17 cells (Th17) play important roles in host immune defense against infection, but uncontrolled activation of these cells, known as the Th17 response, may cause autoimmune and autoinflammatory diseases (uveitis, multiple sclerosis, rheumatoid arthritis, and Crohn’s disease) through the effects of Th17 lineage cytokines (such as, IL-17F, IL-22 and GM-CSF). Importantly, IL-17A (a proinflammatory cytokine) represses other Th17 lineage cytokines by upregulating the regulatory cytokine IL-24. Loss of this regulatory pathway due to IL-17A neutralization, and consequent upregulation of the other Th17 cytokines, may result in reduced efficacy of anti-IL-17A therapy. The inventors suggest that targeting the Th17 lineage cytokines as a class, by augmenting IL-24 may be a better approach for controlling the Th17 response than targeting IL-17A alone, which is currently under development by pharmaceutical companies. For instance, the current strategy to suppress Th17 activity [use of Secukinumab (Cosentyx)] has had only limited success in treating some autoimmune diseases, possibly because reducing IL-17A permits upregulation of other Th17-related proinflammatory cytokines through an intermediate step involving reduced IL-24. Researchers at the National Eye Institute (NEI) have developed a new strategy of using IL-24 to target the whole Th17 lineage and thus achieve improved efficacy in therapy of Th17-relevant autoimmune diseases.
Competitive Advantages:
- Monotherapy of IL-17A targeting alone is insufficient in some diseases
- May avoid patients’ exposure to infections that are possible when targeting both IL-23 and IL-12 combination therapy or STAT3 blockade – as either can be broadly suppressive
- This approach is designed to bring other members of the Th17 pathway back to normal, rather than massively inhibiting them, while targeting its most proinflammatory member IL-17A; the approach augments the naturally produced regulatory cytokine, IL-24, which becomes deficient due to IL-17 neutralization
- Side effects of IL-24 augmentation/normalization are likely to be minimal
- Local treatment to augment IL-24 in the eye reduces inflammation and may reduce systemic side effects
Commercial Applications:
- Potential therapeutic drugs for Th17-relevant inflammatory diseases such as uveitis, arthritis, and multiple sclerosis etc.
- Potential therapeutic drugs for regulating the Th-17 response in various inflammatory conditions
